
Arthritis Consumer Experts National Survey on Artificial Intelligence and Arthritis Care Report
In this issue of JointHealthTM insight
- Why AI in arthritis care matters
- Who responded
- Key Survey findings
- What these Survey results mean for arthritis care in Canada
- Implications for key stakeholders
Artificial intelligence (AI) is changing health care everywhere. From early detection of diseases to predicting flare-ups and supporting clinical decision-making, AI tools are moving from research labs into doctors’ offices, hospitals, and peoples’ homes. Yet when it comes to arthritis – the most common chronic disease in Canada – little is known about how people with arthritis currently interact with AI.
The Arthritis Consumer Experts (ACE) National Survey on AI and Arthritis Care is the first of its kind in Canada. It asked people with arthritis
what they know about AI, what concerns they have, and how they feel about its use in diagnosis, treatment, and daily care. It also explored attitudes toward AI in arthritis research and drug development.
This survey is not about the technology alone. It is about understanding the opinions and worries of people with arthritis to ensure that their voices are heard as new tools are designed and implemented. Without patient input, AI risks deepening inequities or eroding trust. With patient input, AI has the potential to support more timely, personalized, and accessible arthritis care.
Why AI in arthritis care matters
Artificial intelligence is already reshaping the way health systems function. In oncology1, radiology2, and cardiology3, AI algorithms are used to identify disease, recommend treatments, and even predict what happens to a person’s health. In arthritis, researchers are trialling AI to read x-rays for signs of joint damage, predict flare-ups based on patient-reported data, and match people to the therapies most likely to work for them.4,5
Rheumatologists are also now using AI scribe technology – a tool that listens during appointments and automatically creates clinical notes – to document patient-doctor interactions, allowing them to focus on their patients instead of typing. In some Canadian research centres, chatbots – computer programs that can answer questions in a conversation-like way – are being tested to answer arthritis questions or help people prepare for appointments.6
But until now, there has been little information about what people living with arthritis think about AI and its use in their health care. Are they comfortable with AI? Do they trust it? Do they feel prepared to use AI-powered tools in their self-care? And do they believe AI could help with healthcare system challenges, like long wait times for rheumatology appointments or joint replacement surgeries?
The ACE National Survey on AI and Arthritis Care set out to answer these questions. The online survey was open to everyone from June 18 to August 10, 2025, and consisted of 23 questions. More than 282 respondents living with arthritis shared their views, making this the most comprehensive patient-led look at patient perceptions of AI in arthritis care. Their responses tell a powerful story: people are curious, interested, and even hopeful, but they also want oversight, transparency, and fairness.
Who responded
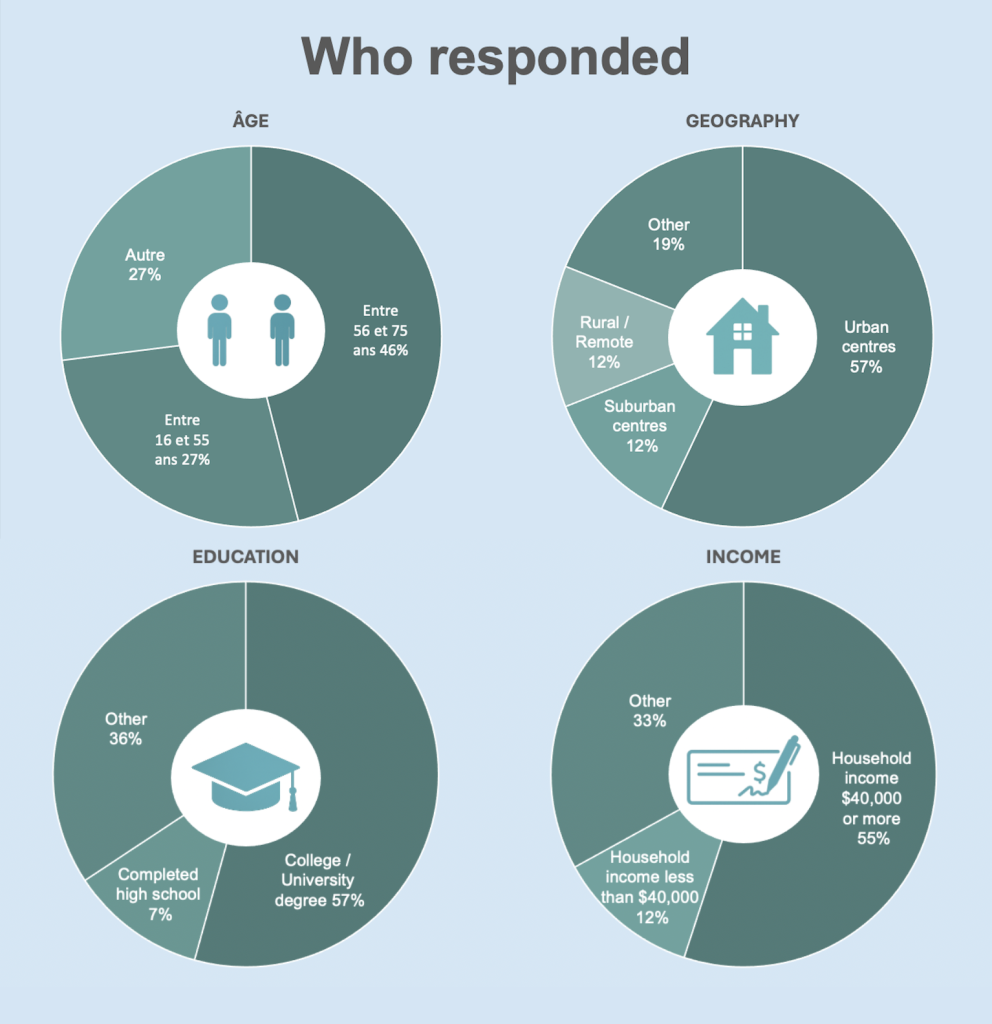
Survey respondents represented the diversity of arthritis in Canada. They included people living with osteoarthritis, rheumatoid arthritis, psoriatic arthritis, lupus, ankylosing spondylitis, vasculitis, and other forms of inflammatory arthritis. Respondents came from every province and territory, with notable participation from both urban centres and rural and remote communities.
Age: Respondents ranged from young adults to older adults, reflecting the full life course of arthritis. Forty-six per cent were between 56-75 and 27% were between 16-55. Approximately 4 out of 10 individuals reported living with their arthritis for 0-10 years, while 5 out of 10 reported living with their arthritis for more than 11 years.
Geography: The majority (57%) of respondents lived in urban centres, followed by 12% who lived in suburban areas. In addition, 12% of respondents were from rural or remote areas – important voices in discussions about digital access and equity.
Income and education: Respondents included people across different income brackets and education levels. More than half of the respondents (57%) had college/university education, while 7% had completed high school. Fifty-five per cent of the respondents had middle-to-higher annual household income ($40,000 or more), while 12% had annual household income of $40,000 or less.
Underserved populations: Approximately 14% of respondents identified as Indigenous, Black, or other racialized groups, providing crucial perspectives on fairness, bias, and inclusion in AI design.
Glossary: Making sense of artificial intelligence
Algorithm
A set of rules or steps that a computer follows to make a decision or solve a problem. In healthcare, algorithms help AI look at patterns in test results or self-reported symptoms to give possible answers.
Artificial intelligence (AI)
A type of technology that can “think”, make predictions, or have conversations.
Bias in AI
When an AI system gives results that are unfair or less accurate for certain groups of people, often because the data it was trained on was not diverse or complete. Patients are especially concerned about bias in ethnocultural identity, gender, and geography.
Chatbot / Virtual assistant
A computer program that can answer questions or provide information in a conversation-like way, either through text or voice (for example, answering arthritis-related questions online).
Generative AI
AI that creates new content or provides answers in plain language (for example, a chatbot that explains arthritis treatment options).
Predictive AI
AI that looks at patterns in your health information to forecast what might happen. For example, warning about a possible flare-up or predicting which medication may work best.
Triage
Sorting patients based on urgency or need. In AI, triage can mean helping to decide who should see a doctor or get surgery first.
Transparency
How clearly a tool explains what it does and how it uses your data. Transparent AI lets patients and doctors understand why it made a specific suggestion.
Key Survey findings
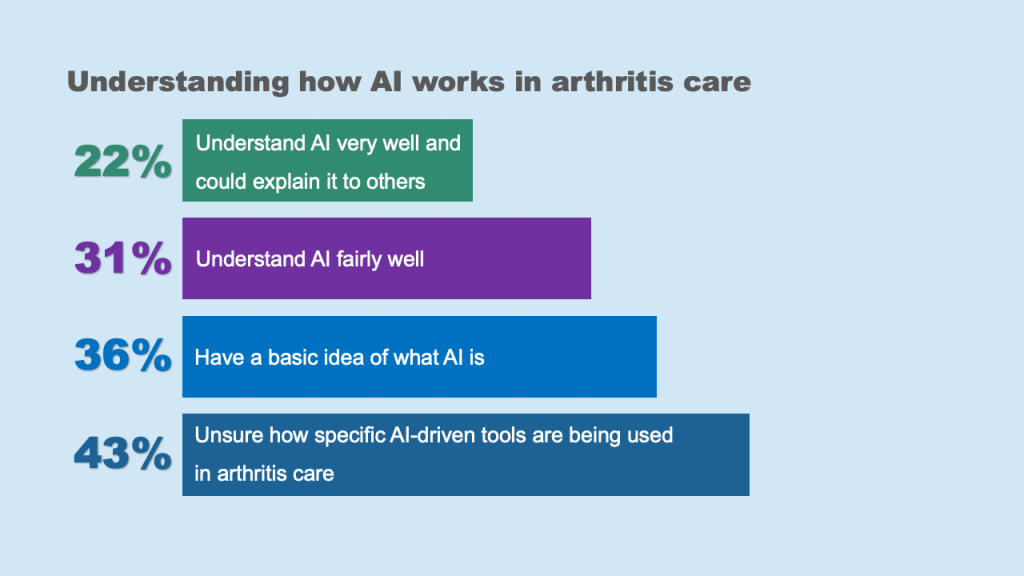
Awareness and understanding
The Survey found that while some respondents were aware that AI exists in healthcare, the majority were unsure how it works in arthritis care.
Most respondents expressed strongest interest in learning more about AI and how it might be used for:
- Arthritis research (80%)
- Self-care (77%)
- Care provided by a health care professional (74%)
- Suggesting medications that best match symptoms and med history (73%)
- Managing waitlist for joint replacement surgery ((65%)
“I have a recent diagnosis and initiation of treatment for GPA and like AI, but have not used for my disease, I didn’t think about it! I want to start now however.”
~ Woman living with Raynaud’s phenomenon, vasculitis, and GPA
The gap between awareness and use is critical. People know AI is out there, but they don’t yet see how it fits into their arthritis care journey. ACE’s Survey findings around awareness and understanding highlight the urgent need for patient education that is clear and accessible to different levels of health and digital literacy. Without it, people may resist AI-driven arthritis care, even if those tools could improve access or outcomes. For example, 65% of respondents were interested in learning more about how AI is helping to manage surgical waitlists, especially for joint replacement and prioritizing cases by urgency, but also wanting assurance there were safeguards to ensure fairness. Twenty-eight per cent of respondents were aware of AI scribes that take notes during appointments, freeing doctors to focus on conversation. However, respondents were concerned about the need for clear consent and data protection.
These findings are consistent with international studies. For example, a 2025 study published in JAMA Network Open (2025) found that when patients saw a physician visibly using AI – whether for diagnostics, administrative, or therapeutic purposes – they perceived the physician as less trustworthy, empathetic, and competent compared to a scenario where AI was not mentioned.7 Arthritis Research Canada’s current ChatRheum research project focusses on a rheumatology chatbot that is trained to answer rheumatology-related questions. Project goals include ensuring the chatbot’s responses are source-verified and measuring how accurate, complete, easy to understand, and compassionate the answers are.

Trust and concerns
Trust is the foundation of any healthcare innovation. Without it, even the most advanced technology will fail to serve patients. Our Survey revealed a complex picture: while many respondents saw promise in AI for health care, their confidence depended on how AI was used and whether a health care provider remained involved.
Respondents expressed higher levels of trust in AI to:
- Make arthritis care more accessible in underserved communities (79%)
- Improve early detection and diagnosis of inflammatory arthritis (75%)
Respondents had less trust in AI to:
- Make accurate assessment about health based on information patient provides (31%)
- Support diagnosis decision-making (30%)
The three concerns most frequently cited by respondents were:
- Inaccurate health information and misdiagnosis (67%)
- Lack of human connection (57%)
- Data privacy (53%)
“I have a recent diagnosis“All patients names and health numbers must be encrypted. Maybe have an air gapped server names and numbers could be held it. Security number one.”
~ Man living with osteoarthritis and chronic pain
“AI is a tool that can be manipulated with time to provide false or incorrect data if a person feeds it misinformation. I worry about the potential negative patient outcomes by becoming too reliant on AI. I worry that patients who are vulnerable and desperate for help or answers may be given wrong or dangerous information by the AI unless it is tightly regulated and closely monitored. I think AI should only be used as a tool to assist the diagnostic and treatment process. I do not believe it should be used in place of highly skilled, educated, competent health care providers.”
~ Woman living with Raynaud’s phenomenon and rheumatoid arthritis
“When fixing the urgency of a knee replacement, I heard the surgeon talking to AI and getting AI replies. I was also involved. But I feel skeptical whether all solutions may be correct. I did raise my concerns to the surgeon who assured me that he is personally involved with his own decisions also and that using AI is only for support and additional assistance.”
~ Woman living with osteoarthritis and diabetes who identifies as a person of colour
The concerns shared by respondents reflect findings from recent studies. Research published July 2025 in JAMA Network Open found that even when AI is used for tasks perceived as non-threatening (like administrative work), it can negatively impact patient perceptions of a physician’s competence, trustworthiness, empathy, and willingness to engage. These effects highlight an important barrier: mentioning AI use, without context or reassurance, can unintentionally erode the patient-physician relationship.7
Use and experience
Despite the media buzz, actual use of AI tools among people with arthritis remains limited. Fifty-one per cent of respondents reported not having used any AI-driven digital health tools. Only a small percentage (27%) of respondents reported knowingly using AI-powered tools in their arthritis care. Among those who had, the most common examples were symptom tracking apps and chatbots answering health questions.
Many respondents reported in their open-ended comments that they had never been informed of the potential use of AI tools by their health care providers. Respondents also commented on barriers to using AI-driven tools, including lack of awareness, lack of access, and concerns about reliability. Respondents commented they are not resistant to technology; they are waiting for it to be offered in a reliable and accessible format. The current lack of use reflects health care system lag, not patient unwillingness to use AI.

“One of my biggest concerns are the possible erosion of medical personnel competency by relying on AI.”
~ Woman living with rheumatoid arthritis who identifies as a person of colour
“I am concerned about the implicit biases that an AI system may hold, especially for equity deserving groups. What checks and balances are in place to ensure that diverse demographics are considered in AI tools? How are we ensuring that AI recommendations are inclusive and equitable? Also, AI tools require an immense amount of energy to run and has climate impacts on our water supply and ecosystem. How are we ensuring that the AI tools used for managing arthritis do not further jeopardize environmental sustainability? Also, what about patients whose first language is not English as most AI tools are English facing there is a systemic barrier there.”
~Woman living with gout and rheumatoid arthritis
“Medical care needs to have a patient centered focus and this needs to be taken into consideration when building the AI model to assess and diagnose patients.”
~ Woman living with Sjögren’s syndrome and dermatomyositis
AI in everyday care
Perhaps the most immediate impact of AI for people with arthritis will be in the everyday care journey, from booking appointments to prioritizing urgent symptoms to supporting recovery after surgery. Our Survey findings highlight both respondents’ support and caution. For example, only 27% of respondents reported they would feel more confident in the safety of a treatment plan if it was developed using AI-driven tools.
When asked what would allow them to feel more confident about the safety of AI-driven tools that are being used in arthritis care, ACE’s Survey found:
- Assurance from health care provider (61%)
- Research and science that supports the use of the AI-driven tools (60%)
- Transparency of the data set that is being used to train the AI (58%)
- Public policies and regulations to protect patients (53%)
- Easy-to-understand instructions (47%)
These views show that people can see the practical benefits of AI, but respondents also are looking for assurances around fairness, privacy, and oversight.
“I think at least a review and discussion with the health care provider to go over the AI recommendations to be sure it is accurate and fits the patient’s individual needs.”
~ Woman living with osteoarthritis in a rural/remote community
“I think AI is an important tool that can be harnessed to assist with patient care. As such, we need to have an open mind as to how it can be developed to enhance health care services whilst acknowledging the fact that human intervention cannot be dismissed entirely. It will be still required to get rid of bias, review assessments and make determinations that AI cannot do, among others.”
~ Woman living with osteoarthritis who identifies as Black
What these Survey results mean for arthritis care in Canada
The results of the first patient-led national Survey on AI and arthritis care in Canada provide a clear message: people with arthritis are open to the use of AI in arthritis care, but only if it is done with transparency, fairness, and human oversight. Across all questions, there was strong consensus that patients and health professionals must remain in control of treatment and care decisions.
ACE’s Survey highlights these challenges moving forward:
- People with arthritis are aware of AI but do not yet see how it fits into their care journey. Without plain-language education and patient-friendly communication, adoption will lag, and inequities in providing health care may worsen.
- Trust in AI depends on oversight, safety, and fairness. People are willing to support AI for diagnostics, research, and even treatment matching – but only if their clinicians remain central and safeguards are built in.
- Differences in awareness, trust, and expectations across race, income, education, and geography show that AI has the power either to close or to widen gaps in arthritis care, but only if it is designed with equity at its core.

Implications for key stakeholders
Artificial intelligence will dramatically continue to change arthritis care over the next five years. Our Survey shows that respondents are not passive recipients of this change and instead have strong opinions, high expectations, and concerns. Taken together, the findings are a call to action for governments, researchers, technology developers, clinicians, and patient organizations. AI will be part of Canada’s healthcare future. The question is whether it will serve all patients fairly or reinforce the biases and barriers to care that already exist.
Implications for governments
Governments must ensure AI tools in arthritis care are regulated for fairness and designed with equity in mind. This includes funding education initiatives that raise awareness and reduce digital divides.
Implications for regulators
People want reassurance that AI-generated drugs or recommendations are tested, peer-reviewed, and human-approved. This means building transparency into drug approval pathways.
Implications for clinicians
Health care professionals should prepare for AI by integrating it into care in ways that support, not replace, their role. Patients trust their providers; that trust must be carried over into AI adoption.

Implications for researchers
Patient willingness to share anonymized data is a tremendous opportunity – but only if patients are partners, not just data sources. Future research must include tests for bias and patients in design, governance, and communication of AI-driven drug trials.
Implications for pharmaceutical manufacturers
Confidence in medications developed using AI was mixed. Some respondents said it would increase their trust, because it implied rigorous analysis of large data sets. Others worried about being “guinea pigs” for untested technologies.
Implications for technology developers
Designing for equity, transparency, and usability will make the difference between adoption and rejection. People with arthritis want plain language, human-centered design, and safeguards.
If you have any questions or would like to learn more about our advocacy efforts, please visit our website at www.jointhealth.org or contact us at feedback@jointhealth.org.

Survey Report References
- Srivastav AK, Singh A, Singh S, Rivers B, Lillard JW Jr., Singh R. Revolutionizing Oncology Through AI: Addressing Cancer Disparities by Improving Screening, Treatment, and Survival Outcomes via Integration of Social Determinants of Health. Cancers. 2025; 17(17):2866. https://doi.org/10.3390/cancers17172866
- Obuchowicz R, Lasek J, Wodziński M, Piórkowski A, Strzelecki M, Nurzynska K. Artificial Intelligence-Empowered Radiology-Current Status and Critical Review. Diagnostics (Basel). 2025 Jan 24;15(3):282. doi: 10.3390/diagnostics15030282. PMID: 39941212; PMCID: PMC11816879.
- Shuja MH, Shakil F, Shuja SH, Hasan M, Edhi M, Abbasi AF, Jawaid A, Shakil S. Harnessing Artificial Intelligence in Cardiology: Advancements in Diagnosis, Treatment, and Patient Care. Heart Views. 2024 Oct-Dec;25(4):241-248. doi: 10.4103/heartviews.heartviews_103_24. Epub 2025 May 10. PMID: 40488153; PMCID: PMC12139645.
- Mondillo G, Colosimo S, Perrotta A, Frattolillo V, Gicchino MF. Unveiling Artificial Intelligence’s Power: Precision, Personalization, and Progress in Rheumatology. J Clin Med. 2024;13(21). doi:10.3390/jcm13216559
- Bilgin Emre. Current application, possibilities, and challenges of artificial intelligence in the management of rheumatoid arthritis, axial spondyloarthritis, and psoriatic arthritis. Ther Adv Musculoskelet Dis. 2025; 17:1759720X251343579. doi:10.1177/1759720X251343579
- Arthritis Research Canada. Current Research: “ChatRheum: Developing a chatbot for answering rheumatology-related patient questions.” https://www.arthritisresearch.ca/research/chatrheum-developing-a-chatbot-for-answering-rheumatology-related-questions/?utm_source=chatgpt.com
- Public Perception of Physicians Who Use Artificial Intelligence. JAMA Network Open. Moritz Reis, Florian Reis, Wilfried Kunde. DOI: 10.1001/jamanetworkopen.2025.21643, https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2836557
Listening to you
We hope you find this information of use. Please tell us what you think by writing to us or emailing us at feedback@jointhealth.org. Through your ongoing and active participation, ACE can make its work more relevant to all Canadians living with arthritis.
Update your email or postal address
Please let us know of any changes by contacting ACE at feedback@jointhealth.org. This will ensure that you continue to receive your free email or print copy of JointHealth™ insight.
Arthritis Consumer Experts (ACE)
Who We Are
Arthritis Consumer Experts (ACE) and its team members acknowledge that they gather and work on the traditional, ancestral and unceded territory of the Coast Salish peoples -ʷməθkʷəy̓əm (Musqueam), Sḵwx̱wú7mesh (Squamish), and Səl̓ílwətaʔ/Selilwitulh (Tsleil-Waututh) Nations.
Arthritis Consumer Experts (ACE) operates as a non-profit and provides free research based education and information to Canadians with arthritis. We help (em)power people living with all forms of arthritis to take control of their disease and to take action in healthcare and research decision making. ACE activities are guided by its members and led by people with arthritis, scientific and medical experts on the ACE Advisory Board. To learn more about ACE, visit www.jointhealth.org
Disclosures
Over the past 12 months, ACE received financial and in-kind support from: Amgen Canada, Arthritis Research Canada, Arthritis Society Canada, Biogen Canada, Canadian Biosimilars Forum, Canadian Rheumatology Association, Celltrion Healthcare Canada, JAMP Pharma, Novartis Canada, Organon Canada, Pfizer Canada, Sandoz Canada, UCB Canada, and the University of British Columbia.
ACE also received unsolicited donations from its community members (people with arthritis) across Canada.
ACE thanks funders for their support to help the nearly 6 million Canadians living with osteoarthritis, rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis and the many other forms of the disease.
Disclaimer
The material contained on this website is provided for general information only. This website should not be relied on to suggest a course of treatment for a particular individual or as a substitute for consultation with qualified health professionals who are familiar with your individual medical needs. Should you have any healthcare related questions, you should contact your physician. You should never disregard medical advice or delay in seeking it because of something you have read on this or any website.
This site may provide links to other Internet sites only for the convenience of World Wide Web users. ACE is not responsible for the availability or content of these external sites, nor does ACE endorse, warrant or guarantee the products, services or information described or offered at these other Internet sites.
Although the information presented on this website is believed to be accurate at the time it is posted, this website could include inaccuracies, typographical errors or out-of-date information. This website may be changed at any time without prior notice.
